Patients over 50 who have been pharmacogenetically tested prior to hospital discharge have a significantly reduced need for emergency department (ED) visits and re-hospitalizations. In a study in the USA, testing reduced ED visits by 42%, hospitalizations by 52%, and ED visits and hospital stays combined by 48% during the two-month follow-up period. The reduction in need for ED visits and hospitalization accounted for estimated savings of approx. $4,000 per patient during the follow-up period. 4
According to a German study, 37% of people over the age of 65 are polypharmacy patients, and 42% regularly use at least one drug that is significantly affected by pharmacogenetics 1. Cardiovascular drugs, painkillers, antidepressants and antipsychotics were among the drugs identified in the study.
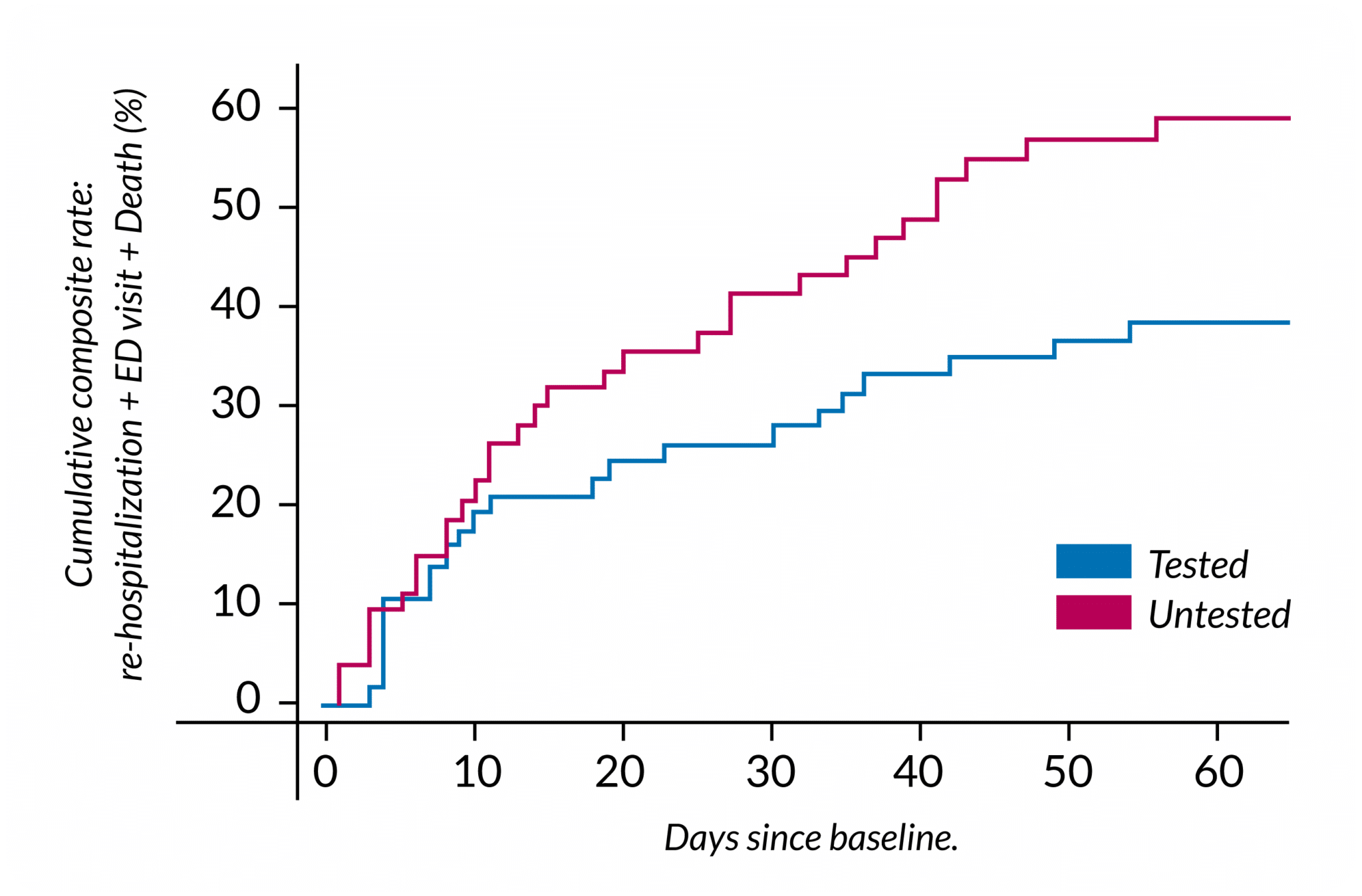
Figure 4 used under CC BY. Adapted from original.
Adverse drug reactions (ADR) cause significant costs to society, and even life-threatening harm to patients. As the number of simultaneous medications increases, so does the risk adverse drug effects. A study in Finland showed that drug-related problems was the certain or probable cause for the ED visit in 16–29% of the ED visits of polypharmacy patients aged 65 or older 6. A study conducted in England found that 89% of people over 70 had been prescribed a drug affected by pharmacogenetics. Correspondingly, 25% had been prescribed at least five drugs that are affected by pharmacogenetics 7.
A pharmacogenetic test can predict the patient’s individual drug response and prevent the use of ineffective drugs. 7
The test results also show whether a drug is more likely to cause adverse effects to the patient at typical dosage. By adjusting the dosage of the drug or changing it to another pharmaceutical if necessary, the doctor can avoid using drugs and dosages that are ineffective for the patient or have a higher risk of side effects.
[1] de Vries, F., Stingl, J. and Breteler, M. (2020) Polypharmacy, potentially inappropriate medication and pharmacogenomics drug exposure in the Rhineland Study. British Journal of Pharmacology. 87(7), 2732-2756. https://doi.org/10.1111/bcp.14671
[2] Kauppila, M. et al (2021) Incidence, preventability, and causality of adverse drug reactions at a university hospital emergency department. European Journal of Clinical Pharmacology. 77, 643-650. https://doi.org/10.1007/s00228-020-03043-3
[3] Brixner, D et al. (2016) The effect of pharmacogenetic profiling with a clinical decision support tool on healthcare resource utilization and estimated costs in the elderly exposed to polypharmacy. Journal of Medical Economics. 19(3), 213-228. https://doi.org/10.3111/13696998.2015.1110160
[4] Elliott, L. (2017) Clinical impact of pharmacogenetic profiling with a clinical decision support tool in polypharmacy home health patients: A prospective pilot randomized controlled trial. PLOS ONE. 12(2), e017905. https://doi.org/10.1371/journal.pone.0170905
[5] Official Statistics of Finland (OSF): Statistics on road traffic accidents [e-publication]. ISSN=2342-3846. 2019. Helsinki: Statistics Finland [referred: 9.11.2022]. Access method: http://www.stat.fi/til/ton/2019/ton_2019_2021-01-19_tie_001_en.html
[6] Schepel, L. et al. (2019) Medication Reconciliation and Review for Older Emergency Patients Requires Improvement in Finland. International Journal of Risk & Safety in Medicine. 30(1), 19-31. https://doi.org/10.3233/JRS-180030
[7] Kimpton, J. E., Carey, I. M., Threapleton, C. J., Robinson, A., Harris, T., Cook, D. G., … & Baker, E. H. (2019). Longitudinal exposure of English primary care patients to pharmacogenomic drugs: an analysis to inform design of pre‐emptive pharmacogenomic testing. British journal of clinical pharmacology, 85(12), 2734-2746. https://doi.org/10.1111/bcp.14100
The amount of scientific data on pharmacogenetics is vast and continuously growing and it can be difficult to stay on top of all the emerging research along with your clinical work. This is why the Abomics pharmacogenetic report compiles all the pharmacogenetic knowledge relevant to the clinician as usage and dosing recommendations of medications. Our team of medical doctors with expertise in pharmacogenetics follow closely all the new research in pharmacogenetics and update the recommendations in the report accordingly so that you can always have recommendations based on the latest research at your hand – without the need to go through all the research papers yourself.
The medication recommendations are based on the synthesis of information gathered by our board of medical advisors. The sources include peer-reviewed scientific literature of high quality, FDA’s (U.S. Food and Drug Administration) list of pharmacogenetic biomarkers in drug labels, EMA (European Medicines Agency), CPIC (Clinical Pharmacogenetics Implementation Consortium), and DPWG (Dutch Pharmacogenetics Working Group). The medication decisions for each patient are up to the treating doctor. The medication decisions for each patient are up to the treating doctor.
The Abomics pharmacogenetic report has recommendations for over 100 medicines based on the patient’s phenotype. We have designed the report especially for e.g., psychiatrists and general practitioners and using it doesn’t require specialisation in genetics. The report is easy to use as a medication decision support tool even during a short doctor’s appointment. The report has a summary of medicines that are significantly affected by the patient’s phenotype and practical guidelines for how to use a medicine for each patient specifically. The digital report is searchable so you can find the patient-specific recommendations easily with the name of the pharmaceutical substance.
Contact us about the availability of the test.

Abomics, Abomics PGx, GeneRx, GeneAccount are registered or non-registered trademarks of Abomics Oy in various countries.