[1] Lääkealan turvallisuus- ja kehittämiskeskus Fimea & Kansaneläkelaitos. (2021) Suomen lääketilasto 2020. Helsinki. https://urn.fi/URN:NBN:fi-fe2021122162417
[2] GeneRx-tietokanta, Abomics Oy https://www.terveysportti.fi/apps/laake/ sekä https://www.terveysportti.fi/apps/generx/
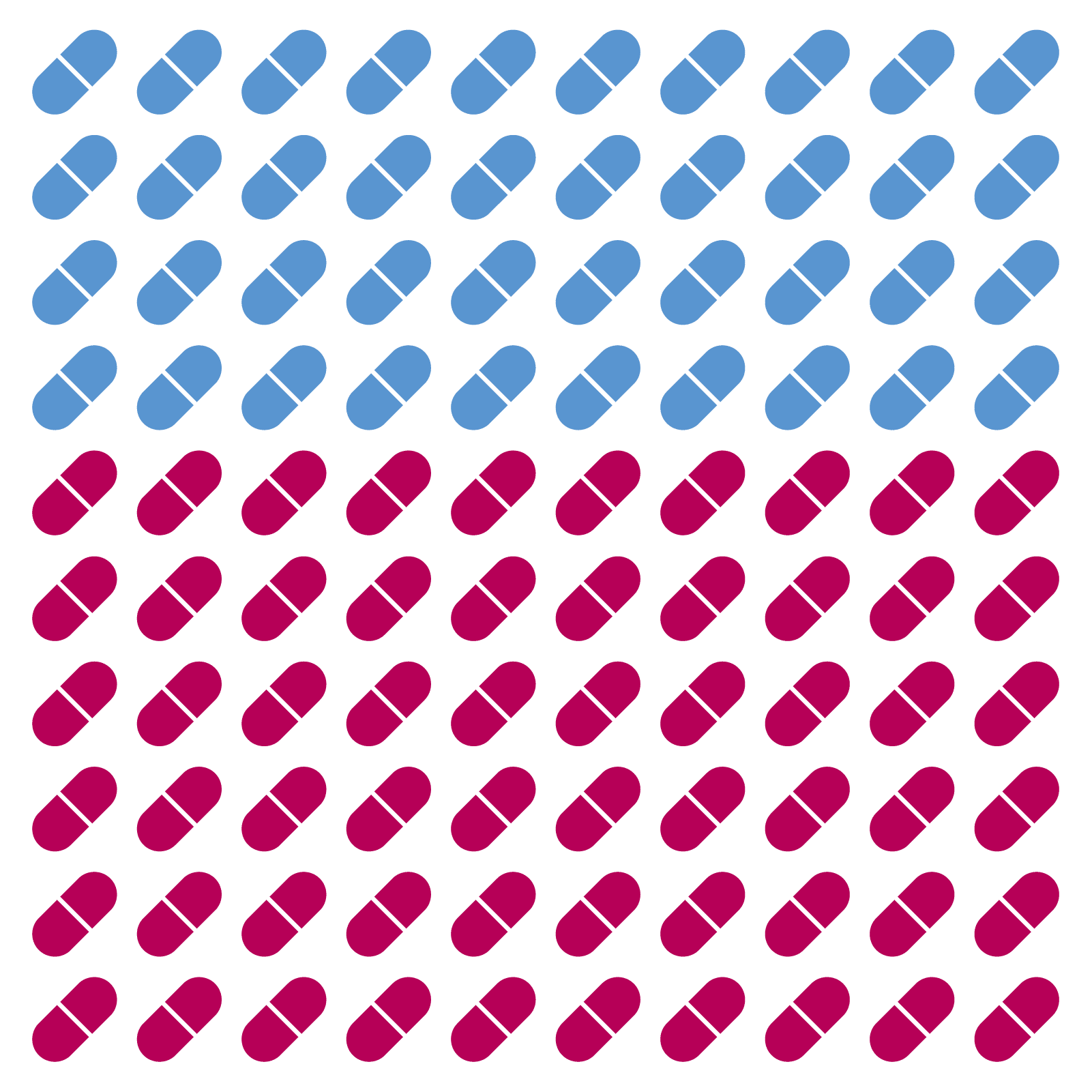
Abomics’ experts maintain a database that includes over 150 pharmaceuticals that are known to be affected by genetic variation and for which a clinically significant recommendation exists. Many of these drugs are widely used. The safety and effectiveness of many antidepressants and antipsychotics is affected by pharmacogenetics.1-2 Several drugs used for treatment of cardiovascular diseases, such as clopidogrel, atorvastatin and warfarin, are also significantly affected by pharmacogenetics.
The effectiveness of some drugs is easy to measure: if the pain isn’t relieved after taking pain medication, the drug doesn’t work. However, measuring the effectiveness of a drug isn’t always this straightforward. For example, the effectiveness of antidepressants can often be evaluated only after several weeks or even months after starting the medication. For some medications such as clopidogrel, which is commonly used to prevent ischemic stroke and heart attack, the effect can only be measured with a laboratory test. With pharmacogenetic testing the doctor knows beforehand how your genetic traits impact different medications and can anticipate whether a medication will work for you or not and how your dosage should be adjusted.
With a personalised medication approach guided by pharmacogenetics, time spent on trial-and-error optimisation can be avoided and the risk of side effects reduced.
[3] Pérez, V. et al. (2017) Efficacy of prospective pharmacogenetic testing in the treatment of major depressive disorder: results of a randomized, double-blind clinical trial. BMC Psychiatry. 17, 250. https://doi.org/10.1186/s12888-017-1412-1
[4] Bradley, P. et al (2018) Improved efficacy with targeted pharmacogenetic-guided treatment of patients with depression and anxiety: A randomized clinical trial demonstrating clinical utility. Journal of Psychiatric Research. 96, 100-107. https://doi.org/10.1016/j.jpsychires.2017.09.024
[5] Bousman, C. et al. (2018) Pharmacogenetic tests and depressive symptom remission: a meta-analysis of randomized controlled trials. Pharmacogenomics. 20(1), 37-47. https://doi.org/10.2217/pgs-2018-0142
[6] Perlis, R. H. et al. (2018) Pharmacogenetic testing among patients with mood and anxiety disorders is associated with decreased utilization and cost: A propensity-score matched study. Depression & Anxiety. 2018; 35: 946– 952. https://doi.org/10.1002/da.22742
[7] Brixner, D. et al. (2016) The effect of pharmacogenetic profiling with a clinical decision support tool on healthcare resource utilization and estimated costs in the elderly exposed to polypharmacy. Journal of Medical Economics. 19(3), 213-228. https://doi.org/10.3111/13696998.2015.1110160
Pharmacogenetics affects drugs used in many therapeutic areas. Scientific evidence supporting the use of pharmacogenetic testing is particularly strong in the treatment of depression, because it reduces adverse drug effects, speeds up recovery and reduces the need of hospitalisation 3-6. Patients with several simultaneous medications also benefit from pharmacogenetic testing as both the need for emergency room care and hospitalisation is decreased 7. Read more about how you could benefit from pharmacogenetic testing.

Abomics, Abomics PGx, GeneRx, GeneAccount are registered or non-registered trademarks of Abomics Oy in various countries.