There are many options available for antidepressant medication, but which will work the best for you? A drug that works for someone else is not necessarily the best drug for you, because our response to drugs is individual and depends on our DNA. In the past, a suitable medication was determined by trial-and-error, which sometimes took a long time. Fortunately, nowadays pharmacogenetic testing can support your doctor in medication decisions. It enables your doctor to rule out medications that are unsuitable for you because of your individual genetic traits. This can not only speed up the process of finding a suitable medication but also decrease your risk of suffering from adverse drug reactions.
The effect of an antidepressant can typically be seen after weeks from starting or changing the medication. When changing the dosing of a drug, it can also take weeks before the effect can be assessed. If a drug is discontinued due to inefficiency or adverse drug reactions, the dose is often lowered gradually over weeks or even months to minimise the possible withdrawal symptoms, further adding up to the time it takes to find a medication that works for you. This means it can sometimes take months before a suitable drug and dose are found and the process of recovery can truly start. Repeated medication changes, medication ineffectiveness or side effects can be frustrating and may sometimes lower motivation and commitment to care and medication.
The choice of an antidepressant is influenced by many factors, which the doctor takes into account when making a medication decision. Pharmacogenetic testing can predict whether a medicine is suitable for you already before trialling it for several weeks. Based on the test results your doctor can choose the most suitable medicine and dose for you individually, which lowers your risk of side effects and long periods of ineffective medications. Patients with depression are often prescribed escitalopram, which is one of the most commonly prescribed antidepressants. However, about 62 % of people have a gene variant, which causes escitalopram to leave the body faster or slower than typical 1. This means that escitalopram with a standard dose only works as expected for fewer than every second patient. A pharmacogenetic test can tell your doctor whether escitalopram is a suitable option for you or not. Based on the test, the doctor can choose a more suitable dose or a different drug for you, and you may be spared several weeks of ineffective medication or unnecessary risks of side effects. Pharmacogenetics has a similar impact on many other common antidepressants, such as citalopram, amitriptyline and venlafaxine.
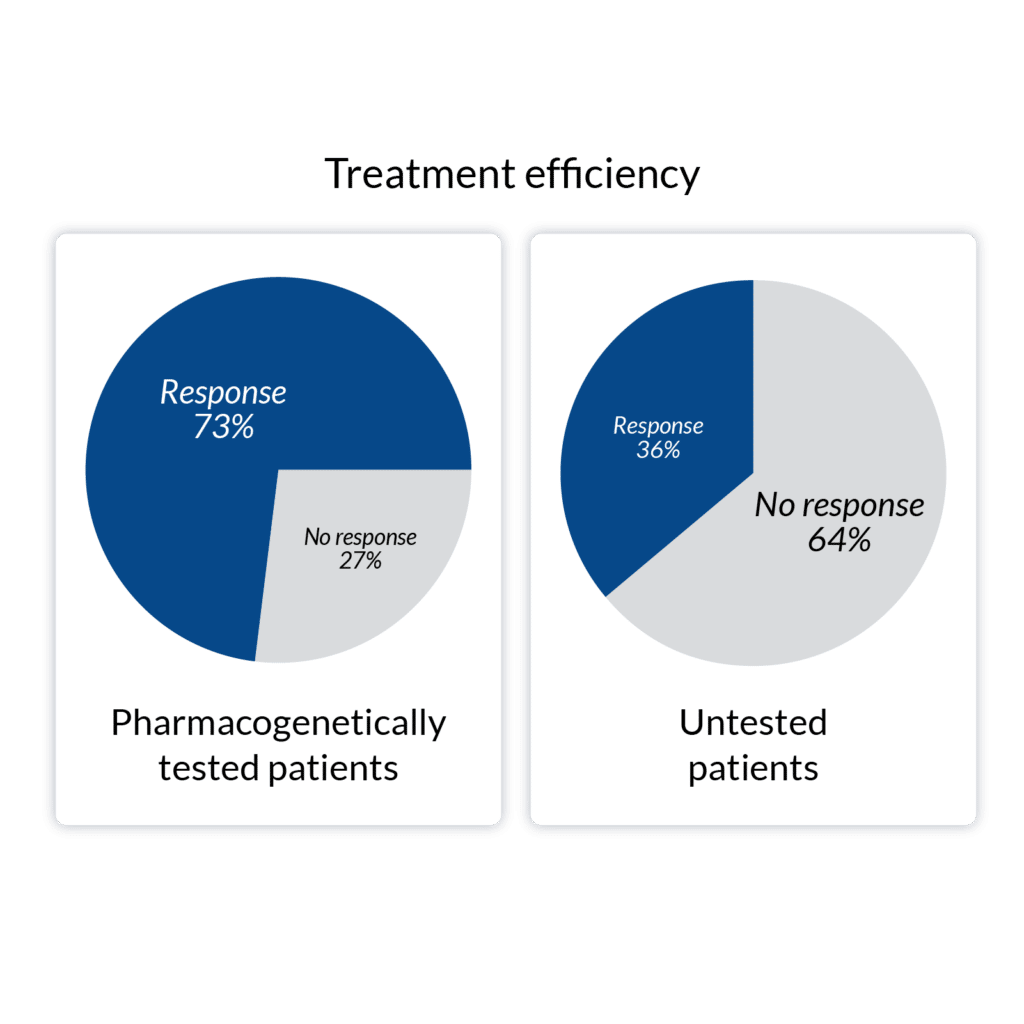
In a study of patients with severe depression, 73 % achieved a drug response* in 12 weeks when pharmacogenetic test results were available for the doctor. Without the test results only 36 % of the patients achieved drug response in the same time period.2 Pharmacogenetic testing has also been shown to decrease the number of emergency room visits and hospitalisations of mental health patients 3.
[1] Häkkinen, K. et al. (2022) Implementation of CYP2D6 copy-number imputation panel and frequency of key pharmacogenetic variants in Finnish individuals with a psychotic disorder. The Pharmacogenomics Journal. 22, 166-172. https://doi.org/10.1038/s41397-022-00270-y
[2] Bradley, P. et al. (2018) Improved efficacy with targeted pharmacogenetic-guided treatment of patients with depression and anxiety: A randomized clinical trial demonstrating clinical utility. Journal of Psychiatric Research. 96, 100-107. https://doi.org/10.1016/j.jpsychires.2017.09.024
[3] Perlis, R. H. et al. (2018) Pharmacogenetic testing among patients with mood and anxiety disorders is associated with decreased utilization and cost: A propensity-score matched study. Depression & Anxiety. 2018; 35: 946– 952. https://doi.org/10.1002/da.22742

Abomics, Abomics PGx, GeneRx, GeneAccount are registered or non-registered trademarks of Abomics Oy in various countries.